

Some older adults may sometimes have pseudo-dementia, in which they present with dementia-like symptoms that are caused by depression rather than dementia. They’re used on concussion patients to measure their injury, and can identify neurodevelopmental disorders like attention deficit hyperactivity disorder (ADHD). They can also identify how epilepsy is affecting brain function, or if someone had a stroke in the brain’s left hemisphere. Sometimes they show someone is dealing with mild cognitive impairment, a precursor to dementia, or different types of dementia. Neuropsychological assessments yield different results depending on the patient, says LeMonda. Those patterns can shed light on what part of the brain may be functioning suboptimally - and that informs what the diagnosis might be. The results for these types of extensive exams are then compared to data representative of people with the same age, gender, and years of education, according to McEwen.Įach individual test doesn’t indicate whether someone has a cognitive impairment, but rather the neuropsychologist looks for certain patterns across all the tests administered. “A true neuropsychological evaluation will also look at mood components and personality components that can influence our cognitive functioning,” LeMonda said. They can also look at how someone’s mood affects their cognition. These assessments, which can only be accessed by a licensed clinician, can take anywhere from 3 to 7 hours and involve a wide variety of brain functioning tasks: attention, motor skills, spatial functioning, reasoning skills, working memory, learning, language, and recall.

LeMonda says these are “much more thorough, comprehensive standardized assessments” that must be completed by a trained brain behavior professional. This is far different from a simple cognitive test. The gold standard for evaluating a person’s cognitive state is a neuropsychological assessment, according to LeMonda. How do neuropsychological assessments work? If someone performs well, it doesn’t necessarily rule out an underlying brain issue, because the cut-off scores are so high,” LeMonda told Healthline.īecause the tests are so basic, a high score doesn’t always mean there are no impairments, LeMonda adds.Ĭognitive screening measures like the MoCA also don’t reveal why the impairment is there or exactly where it is.
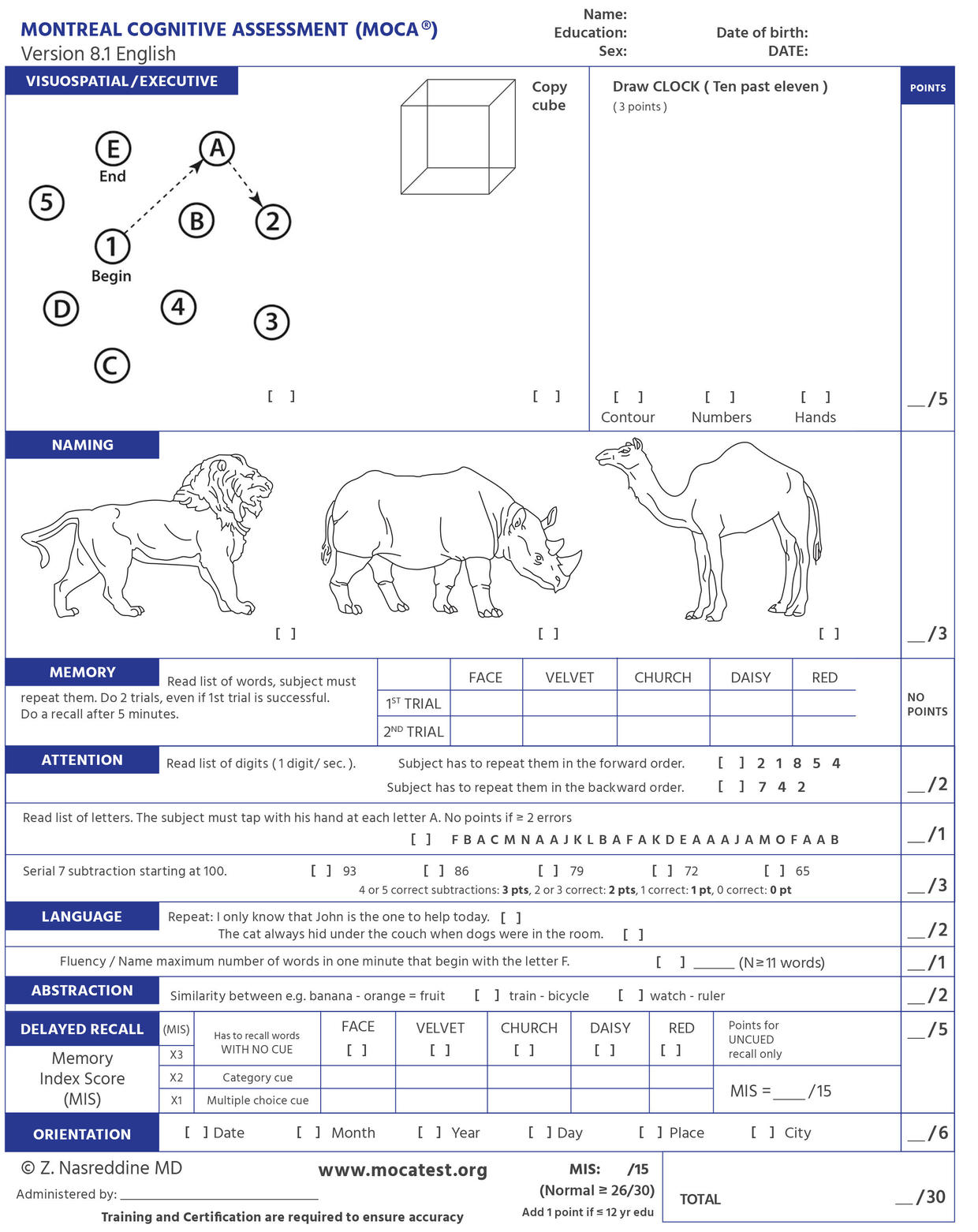
“If someone performs poorly, then that’s really an indication that there’s some kind of brain dysfunction. The threshold for gauging any sort of dysfunction is so low, according to LeMonda, that the tests don’t give too much insight into what’s going on. Past research suggests they shouldn’t be used alone to diagnose neurodegenerative disorders. “There are standardized scores for these tests, which illuminate if an impairment in one or more cognitive domains is significant and warrants further testing and treatment planning,” said Sarah McEwen, PhD, director of research and programming for the Pacific Neuroscience Institute at Providence Saint John’s Health Center. Screening tests are mostly used to quickly determine whether someone has any brain dysfunction and if they need additional diagnostic testing. The Mini-Cog and MMSE are two other quick screening tests used to determine whether someone’s cognition may be off due to a health issue like dementia, delirium, stroke, or even a head injury.īrittany LeMonda, PhD, a senior neuropsychologist at Lenox Hill Hospital in New York City, says these sorts of tests are often administered in hospital settings by a nurse or physician who may not always have a background in brain sciences. The MoCA typically takes around 10 minutes and involves simplistic tasks designed to screen for impairment in an individual. What are cognitive screening tests, like the MoCA?


 0 kommentar(er)
0 kommentar(er)
